The #1 Key for Hospital Administrators and Exceptional Patient Outcomes
Hospitals across the country are constantly having to adapt to change. One of the most recent changes is that hospitals will now be rewarded for patient care rather than patient volume. USA Today recently reported that under the Affordable Care Act, “the government will offer financial incentives to hospitals that perform well. The government determines good performance through a combination of clinical outcomes and patient satisfaction surveys. The Affordable Care Act also will penalize hospitals that perform poorly.”
With the potential for significant financial losses for reimbursements for hospitals that fail to meet patient satisfaction and quality clinical care outcomes, employee engagement is more important than ever. However, many of today”s hospitals lack leadership and staff development programs, and now employee engagement is “code blue.” The losses could total millions of dollars for some hospital systems that receive funding from government reimbursements.
Based on our experience in training over 100 hospital administrators and clinical leaders in roughly 50 hospitals and surgical centers across the U.S., patient outcomes are extremely dependent on motivation, communication, devotion and exceptional customer service skills of hospital staff and physicians.
How can hospital administrators start preparing to adapt successfully and engage their staff to create exceptional patient experiences and outcomes?
Determine a patient experience strategy
The average hospital has a mission statement, which describes what a hospital does (provide care) and for who it provides care for (patients/local community) but we”ve found that many hospitals have no strategic vision that outlines where their hospital will be within the next five years. The advantage of having a strategic vision is it helps hospitals clearly define and communicate their goals and focuses the entire staff”s efforts toward meeting specific expectations and achieving desired outcomes.
Exceptional Patient Experience = (Staff Engagement Physician Engagement)
Staff Engagement and Retention
The first part of the strategy should focus on fully engaging and retaining hospital staff. In a Towers Watson’s health care engagement study, only 34% of hospital workers stated they go the extra mile or “above and beyond” to exceed expectations. In addition, 42% of hospital workers are partially engaged or more simply put they just “go through the motions.” While their physical bodies may be present, their hearts are not in their work. If hospitals can engage and retain talented staff to perform their best, their actions will positively impact physician relationships and ultimately patient outcomes.
What is employee engagement? We define employee engagement as the strength of the emotional connection and devotion employees have to an organization. Engaging staff requires effective leadership. Hospitals must ensure their mid-level supervisors and managers lead by example, provide praise and recognition at least weekly, cultivate an environment of open communication, trust and respect.
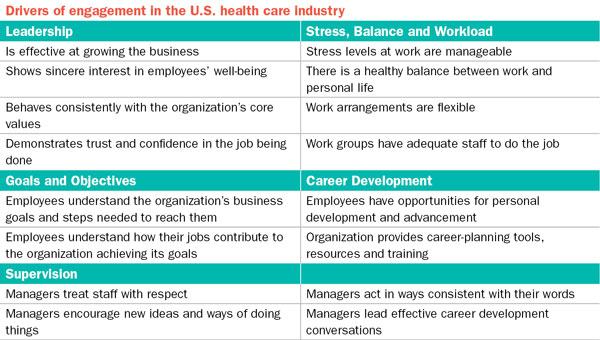 Source: Towers Watson
Source: Towers Watson
The current national average turnover rate for hospitals is roughly 15%. Hospital administrators should calculate and compare their turnover rates to ensure people are not leaving due to poor leadership. As many seasoned authentic leaders know, people don”t typically quit jobs, they usually quit supervisors, managers and toxic work environments.
According to Nursing Solutions Inc., 89.5% of hospitals believe staff retention is a “key strategic imperative,” but it is not made a priority or practiced in day-to-day operations and leadership planning, since 51% of hospitals have no formal staff retention strategy. The best staff retention tool is hiring, training and equipping effective leaders.
Physician Engagement
The second part of the strategy is physician engagement. Health care reform laws will require increased communication, teamwork and coordination between hospital administrators and physician leaders to ensure the best possible outcomes for patients. Unfortunately, most physicians are not taught leadership skills in medical school, residency, or fellowship. Instead, they learn leadership and communication skills as they go over time. A significant part of leadership is knowing how to communicate effectively. Many physicians who have never received formal leadership and communication training, typically communicate based on their feelings and they tend to be aggressive, passive aggressive, and personalize conflicts and disagreements.
According to Dr. Ken Cohn, a practicing surgeon and CEO, he interviewed MBA students and physicians and asked them what percentage of their grade during training was based on team projects. The MBAs said 30 to 50%; the physicians said zero, which concluded his findings that many physicians have never had any formal lessons in communication, team work or negotiation, which is the primary reason so many have autonomous rather than team mindsets.
Becker”s Hospital Review recently reported that hospitals can help develop physicians and strengthen relationships between physicians, administrators and staff by focusing on physician leadership training. The article stated, “hospitals can provide mentoring, education and workshops or bring in outside consultants to help develop physician leaders, which will ultimately lead to the success of the new delivery patient care models.”
What will separate mediocre hospitals from high performing hospitals going forward in 2014 will be hospital administrators ability to develop a strategic vision for creating exceptional patient experiences and their ability to fully engage staff and physicians to execute the vision and make it sustainable.